Medicare vs. Medicaid – Differences Easily Explained
What is Medicaid in the United States?
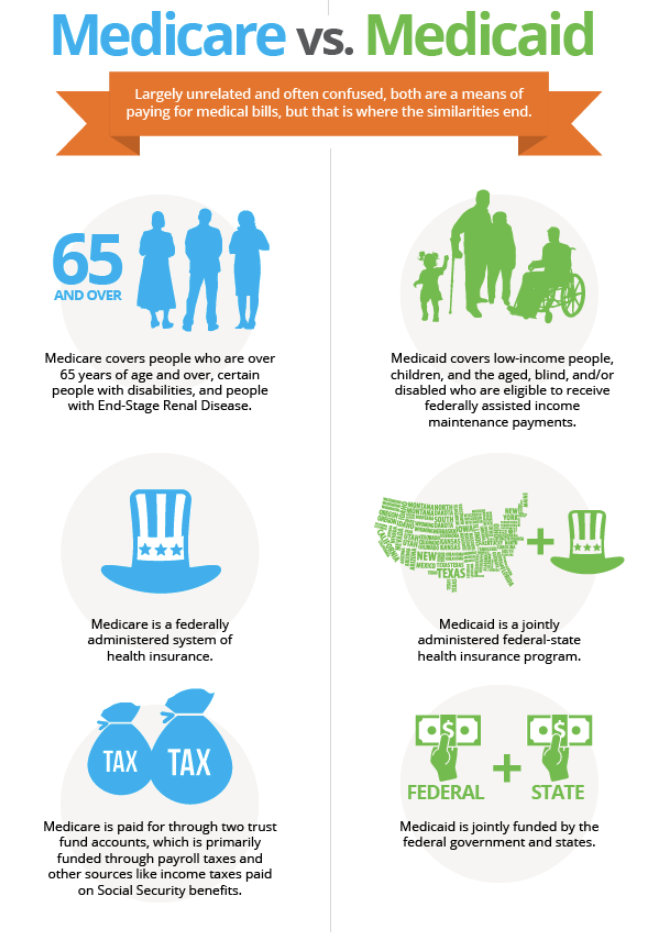
Medicaid is a U.S. Government health insurance program for people in need. U.S. President Lyndon B. Johnson established Medicaid, a part of the Social Security Act.1 Medicaid and the Children’s Health Insurance Program (CHIP) serve more than 31 million children. A national health care program for low-income individuals and families governed jointly by the states and the federal government.
AND
What is Medicare in the United States?
Medicare is a social security coverage program administered by the U.S. government, which provides health care to all people 65 years of age or older who are considered disabled due to serious health problems, such as cancer, kidney failure with need for dialysis, etc. The program also funds training programs for physicians residing in the United States. Medicare operates as an insurance for individuals. A national health insurance program for people over 65 or under 65 with qualifying disabilities.
When looking at care options for older people, many people have questions about how Medicare and Medicaid are involved, and what the main differences are. Here’s a quick snapshot of how the two differ in hopes of clearing up some of the confusion surrounding this issue.
What is Medicare? What does Medicare cover?
- A public benefit that is NOT “need-based”: This means that Medicaid is only available to people who have incomes below the government’s threshold and/or who only have a certain number of assets.
- If a person has been hospitalized for 3 days, they become eligible for Medicare
- Medicare will pay for up to 90 days of hospital care
- After the first 20 days in a hospital, a co-payment is required
- Medicare will also pay for 100 days of skilled nursing care (copayment required after 20 days)
What is Medicaid? What does Medicaid cover?
- Medicaid is also a public benefit, but it IS “need-based
- Medicaid is what you will need if your hospital stay exceeds 100 days, primarily nursing home care
- To qualify, most people need asset planning (managing their assets/ funds) to make sure that their income level is enough to qualify and their asset level is low enough to qualify
- There are a number of tools like this article on asset spending and this Medicaid planning report that advocates use to help you qualify for Medicaid without running out of resources


The Basics of Medicare
Eligibility
The eligibility requirements for Medicare changed over the years as more people were recognized as having a disability and more people were qualified. Income is not a consideration in qualifying for Medicare if you worked and paid into the program.
Anyone over 65 who has worked and paid into Medicare for at least ten years is eligible for Part A (hospitalization – inpatient).
Any person who receives Social Security disability payments for at least 24 months (SSDI).
People with End Stage Renal Disease (ESRD).
People with ALS/Lou Gehrig’s disease (amyotrophic lateral sclerosis).
Any person receiving a Disability Pension from the Railway Retirement Board (RRB)
Benefits
Medicare benefits do not vary. They are the same for everyone
What does it cost you?
Everyone pays a Part B premium, even if they have a Medicare Advantage Plan. Some Advantage Plans have varying premiums and deductibles, some have only one deductible. If you choose ‘original’ Medicare, you will pay a premium for Part B and Part D if you choose to buy it. There will be an additional premium if you choose a Part F supplement.
The Basics of Medicaid
Eligibility
Initially, only people receiving monetary assistance or “social assistance” were eligible. Today, the following groups are eligible:
No income individuals or families
Low-income individuals or families
Pregnant women
People with disabilities regardless of age.
People who need long-term care.
All of these groups had to pass a means test to be eligible. After the passage of the Affordable Care Act, states were allowed to make their financial means equal to 138% of the federal poverty level. States were allowed to opt out and almost half did so. In those states, you must be on the FPL or less.
Benefits
Benefits vary from state to state as each determines which benefits are most needed by people in their state. In most states, children receive the most comprehensive benefits. Benefits for adults vary greatly from state to state.
What does it cost you?
This also varies from state to state. Some states charge high deductibles, while other states do not charge a deductible at all. This again could be linked to a means test. There are many service providers that will not provide services for Medicaid payment. Those with Medicaid have fewer provider choices than those with Medicare.
